AIMS
• Understand normal fluids electrolyte requirements/ maintenance
• Understand how to assess DEHYDRATION in children
• Understand the difference between DEHYDRATION and SHOCK but that they may occur together
MAINTENANCE FLUIDS
RCH FLUID CALCULATOR
Fluid & Electrolytes
Normal Fluid Requirements
INSENSIBLE LOSSES
• Caloric content of feeds
• Ambient temperature
• humidity of inspired air
• Fever
• Stool output usually between 0 -10 ml/kg/day are lost in stools (may exceed 300 ml/kg/day in diarrhoea)
• Urinary output usually between 1-2 ml/kg/hour
Fluid & Electrolytes
Normal Electrolyte Requirements
DEHYDRATION
A condition caused by the excessive loss (deficit) of water from the body
DEGREE OF DEHYDRATION
What are the symptoms and signs of dehydration?
How do you distinguish MILD v MODERATE v SEVERE dehydration?
WEIGHT
• Weigh bare child and compare with any recent (within 2 weeks) weight recordings
• The best method relies on the difference between the current body weight and the immediate pre-morbid weight.
MILD DEHYDRATION <4%
• No clinical signs
• They may have increased thirst
• They will have a history of losses eg vomiting, diarrhoea, increased insensible losses
– DOCUMENT FREQUENCY/ VOLUME/ DURATION OF LOSSES
MODERATE DEHYDRATION 4-6%
• HISTORY OF LOSSES +/ DECREASED URINE OUTPUT
• Central Capillary Refill Time> 2 secs
• Increased respiratory rate
• Mild decreased tissue turgor
• Sunken eyes, fontanelle
• Dry mucous membranes
SEVERE DEHYDRATION > 7%
• HISTORY OF LOSSES, decreased urine output +/- lethargy
• CRT > 3 secs
• Mottled skin
• Decreased tissue turgor
• Other signs of shock
– Tachycardia
– Neurological: irritable or reduced conscious level,
– Hypotension
• Deep, acidotic breathing
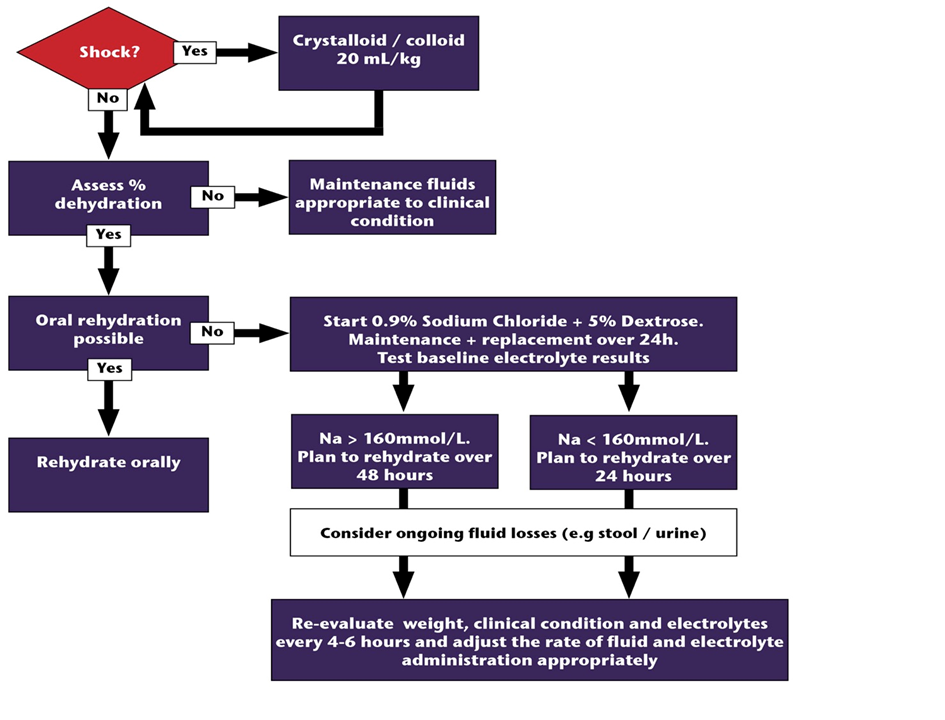
Considering fluids:
Degree of dehydration (deficit) +
Maintenance fluid requirements +
Ongoing losses
Calculate deficit
• Degree of dehydration expressed as % of body weight
– e.g. a 10kg child who is 5% dehydrated has a water deficit of 500mls
– WEIGHT X DEFICIT % X 10 (in ml)
– = 10 X 5 X 10 = 500 ML
• The deficit is replaced over a time period that varies according to the child's condition. Precise calculations (eg 4.5%) are not necessary
• The rate of rehydration should be adjusted with ongoing assessment of the child.
Speed of replacement
• Replacement may be rapid in most cases of gastroenteritis (best achieved by oral or ng fluids)
• SLOWER in DKA, meningitis and HYPERNATRAEMIA
– In Hypernatraemia aim to rehydrate over 48 hours with Na not falling more than 1mmol/litre/hour
SHOCK
Shock occurs as result of rapid loss of 20 mL/kg from the intravascular space
SHOCK
• The treatment of shock requires rapid administration of a bolus of intravascular fluid (start with 10- 20ml/kg then reassess) with electrolyte content that approximates to plasma (eg. 0.9% saline)
• If the intravascular volume is maintained, clinical dehydration is only evident after losses of >25 mL/kg of total body water.
DEHYDRATED BUT NOT SHOCKED
• The treatment of dehydration requires gradual replacement of fluids, with electrolyte content that relates to the to the electrolyte losses, or to the total body electrolyte content.